PubMed is probably the most used search tool in the medical world. As such we are often asked how does Trip differ from PubMed? Or, put it another way, why should we bother with Trip? If you ask ChatGPT it states:
“The Trip Database is a clinical search engine focused on delivering evidence-based summaries, guidelines, and tools for healthcare professionals, making it user-friendly for clinical decision-making. PubMed, by contrast, is a comprehensive repository of biomedical research articles, aimed at researchers and clinicians needing in-depth primary studies. Trip emphasizes practical application, while PubMed is broader and research-oriented.“
But, practically how does this manifest itself? Below is an example that can illustrate the differences. The search stems from a likely clinician question. Trip is focussed on clinical decision making so we focus on the clinical question scenario. As ChatGPT states, PubMed’s aim is broader – so has to accommodate more diverse needs.
Prostate Cancer Screening
Here are the top 3 side-by-side (Trip on the left-hand side):
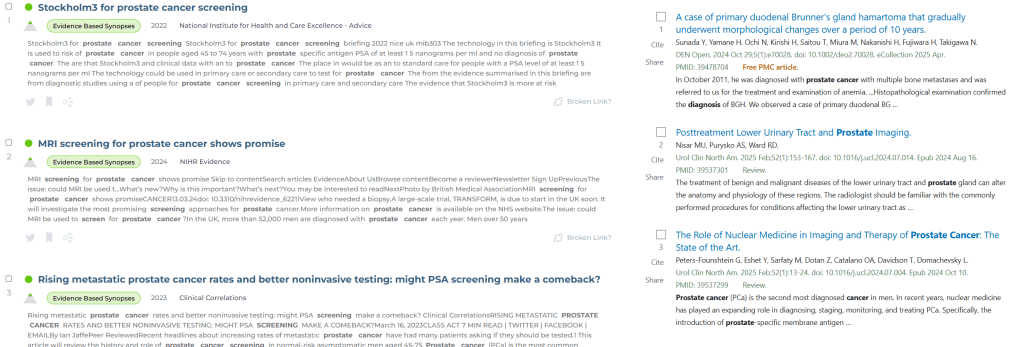
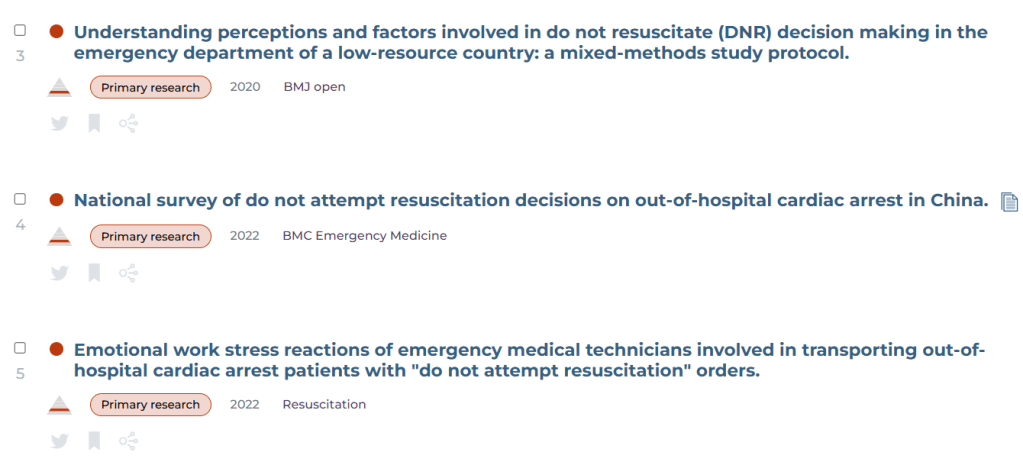
The top three from Trip are all secondary evidence ie higher quality compared to PubMed’s. One of PubMed’s article is a case report and two are about imaging. Below is the top ten:
We asked ChatGPT to compare the results and from the perspective of a busy health professional with a clinical question relating to prostate cancer screening that affects patient care. We also asked it to consider the quality of the evidence.
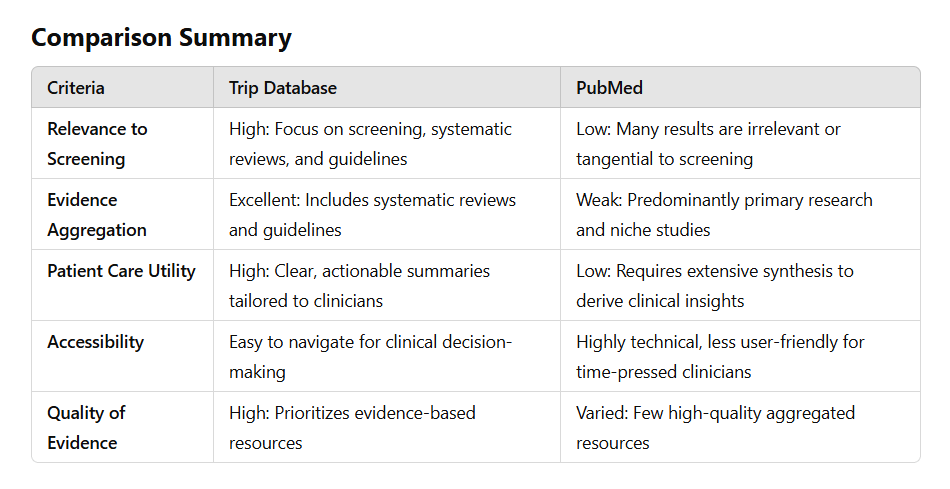
It concluded: “For a busy health professional addressing a clinical question about prostate cancer screening, Trip Database provides a more focused, clinically actionable, and evidence-based set of results. Its emphasis on guidelines and systematic reviews ensures better support for patient care. In contrast, PubMed excels in breadth and niche research but lacks the specificity and usability required for immediate clinical decision-making.“
Pretty clear….
We will continue to generate these comparisons, it’s useful to help explain the strengths of Trip
Recent Comments